The use of Artificial Generative Intelligence systems by healthcare professionals must become widespread; it would be unethical to do without the help of these tools.
Ethical principle of the French Academy of Medicine (translation). Generative AI systems in healthcare: challenges and prospects, 5 March 2024.
This month’s theme: Organ-on-a-chip
Introduction
Organ-on-a-chip (OOC) is a technology that involves the creation of microfluidic cell culture devices that simulate the activities, mechanics, and physiological responses of entire organs or organ systems.
These chips typically contain small chambers lined with living cells that mimic the structure and function of specific organs, such as the heart, liver, lung, or kidney. The purpose of organ-on-a-chip technology is to provide a more accurate model of human physiology compared to traditional 2D cell cultures or animal testing.
By recreating the microenvironment of an organ, including factors like fluid flow, mechanical forces, and cell-cell interactions, researchers can study disease mechanisms, test drug efficacy and toxicity, and even personalize medicine. Each chip can replicate certain functions of its corresponding organ, allowing researchers to study interactions between different organs and systems in the body, known as « body-on-a-chip » systems. This technology has the potential to accelerate drug discovery, toxicology testing, and personalized medicine by offering more reliable and relevant models for studying human biology and disease. Some aspects related to aging have been studied, but following interactions between organs on a long-term scheme and with senescence aspects is still to be done.
The difference between an organ on a chip and an organoid is that OOCs are microfluidic devices mimicking entire organs’ physiological responses, offering precise control over microenvironments for drug testing and disease modeling whereas the organoids are 3D cell clusters derived from stem cells, replicate specific organs’ structures and functions, serving as valuable tools for studying development, diseases, and personalized medicine, albeit with less control over microenvironments
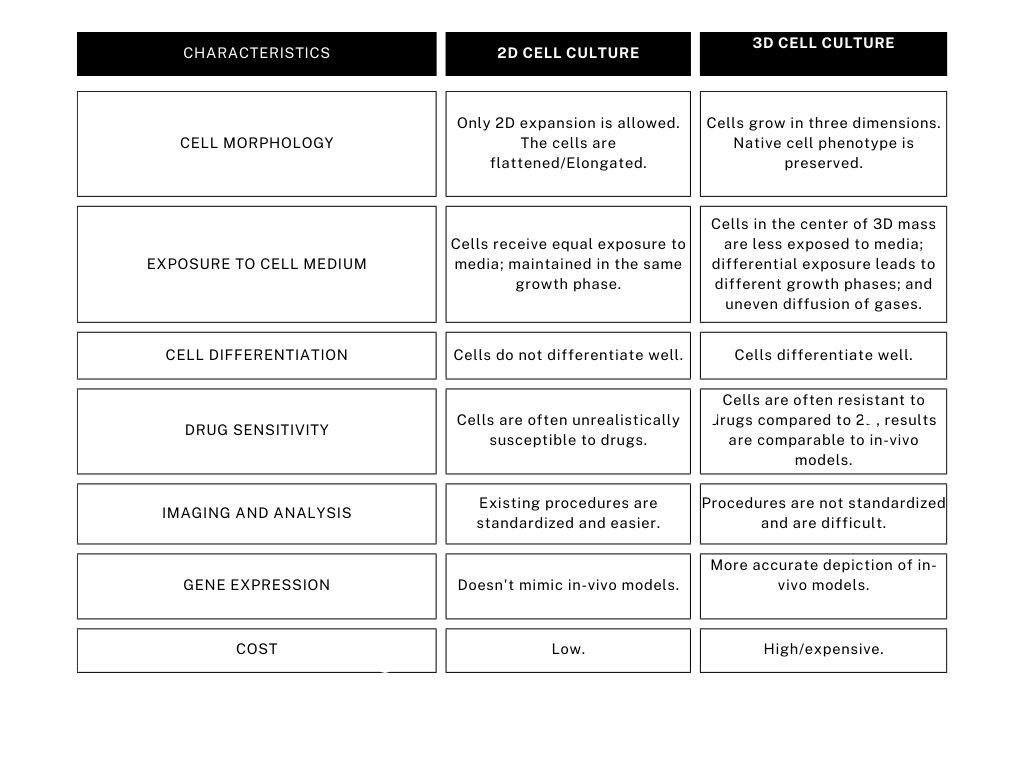
Comparison of characteristics of 2D and 3D cell cultures
Types of Organ-on-a-chip
Lung
A study from 2021 shows that the lung-on-a-chip technology utilizes a biological, stretchable, and biodegradable membrane composed of collagen and elastin, simulating an array of miniature alveoli with dimensions akin to those found in vivo. This membrane undergoes biodegradation, and can be easily customized in terms of thickness, composition, and stiffness through a straightforward manufacturing process. The air-blood barrier is reconstructed using primary lung alveolar epithelial cells sourced from patients alongside primary lung endothelial cells. Notably, the membrane maintains typical alveolar epithelial cell markers and preserves barrier properties for up to three weeks.
Kidney
By utilizing kidney-on-a-chip technology, researchers can replicate physiological conditions found in human organs. Various kidney-on-a-chip models have been created to mimic the microenvironment of the kidney tubule, demonstrating improved accuracy in predicting drug nephrotoxicity compared to traditional methods. Using kidney-on-a-chip platforms, researchers can assess diverse drug-induced biological responses. In the future, the integration of kidney-on-a-chip into multi-organ systems is anticipated. Furthermore, kidney-on-a-chip holds promise for disease modeling and advancing the development of novel renal replacement therapies.
Pancreas
The Pancreas-on-a-chip platform emulates the native functionality and cellular interactions of pancreatic cells more accurately than conventional human cell culture models. This chip facilitates the replication of fluid flow dynamics observed in vivo. Utilizing the Pancreas-on-a-chip has contributed to addressing a fundamental question in cystic fibrosis-related diabetes (CFRD): whether the loss of Cystic Fibrosis(CFTR) function in pancreatic duct epithelial cells (PDECs) is a primary factor in CFRD development. A study suggests that indeed, CFTR dysfunction in PDECs is a significant contributor to CFRD onset.
Heart
Cardiovascular diseases (CVD) stand as the primary cause of mortality in numerous countries. However, the development of cardiovascular drugs faces significant hurdles: (a) Animal models for CVD often inadequately predict human responses; (b) Adverse effects vary between organisms; and (c) The process is lengthy and costly. Organs-on-a-chip technologies have been proposed to mimic the dynamic conditions of the cardiovascular system particularly, the heart and general vasculature. These systems pay particular attention to mimicking structural organization, shear stress, transmural pressure, mechanical stretching, and electrical stimulation.
A beating heart-on-a-chip has been engineered with highly functional micro-engineered cardiac tissues, enabling the prediction of hypertrophic changes in cardiac cells. This innovative device demonstrates the capacity to produce cardiac microtissues with enhanced mechanical and electrical coupling among neighboring cells. Furthermore, the model exhibits a positive chronotropic effect when exposed to isoprenaline, suggesting its potential utility in drug discovery and toxicity studies.
Companies involved in developing the technology
Several major companies are leading the development of organ-on-a-chip models across the globe. In Europe, we have Mimetas, headquartered in the Netherlands, which offers a wide range of organ-on-a-chip models including kidney, gut, tumors, and others. Elvesys, based in France, focuses on developing microfluidic systems. AlveoliX, located in Switzerland, specializes in human lung-on-a-chip models. TissUse, based in Germany, offers multi-organ-on-a-chip solutions. Lastly, BiomimX, headquartered in Italy, is renowned for its expertise in generating predictive models of human organs and pathologies for drug testing.
Emulate, one of the leading companies in the field, is based in the U.S. and specializes in creating advanced models such as lungs-on-chip, gut-on-chip, and blood-brain-barrier-on-chip systems. AxoSim, based in the U.S., is dedicated to creating specialized microfluidic chips for combating cancer. TaraBiosystems, another U.S.-based company, is known for its focus on heart-on-a-chip models. Nortis Bio, based in the U.S., specializes in kidney-on-a-chip models. BioIVT, also headquartered in the U.S., provides established models such as pancreatic islets and lung airway epithelium.
Use of Organ on a chip in longevity studies
Organoids and microfluidic chip technology represent significant advances in molecular biology. Organoids, miniature models of organs generated from stem cells, effectively mimic the morphology and function of actual organs. On the other hand, organs-on-chips employ intricately carved tunnels on plastic or polymer surfaces to house cells, stimulating blood flow within the human body. These technologies have emerged as solutions to the challenges of drug development, which is often slow, costly, and prone to failure due to inadequate predictive tools. By combining organoids and organs-on-chips into « organoids-on-chips, » researchers can leverage the biological accuracy of organoids with the dynamic capabilities of microfluidic chips, enabling a more accurate study of disease traits and drug responses. For instance, integrating a functional vascular system into organoids enhances their complexity and physiological relevanceThe potential of organoids-on-chips extends beyond drug screening to applications in regenerative medicine and fundamental biological research. These technologies could revolutionize medical research and drug development practices, potentially replacing animal testing in toxicology studies and developing personalized therapies.
BIOFABICS, a Portuguese start-up funded by the European Union’s Horizon 2020 research and innovation program, is pioneering custom design tools for bio-fabrication, particularly in the emerging field of organ-on-chip (OOC) technology. The goal of the company is to leverage automated customization processes, allowing users to create large arrays of interconnected organ models. Currently, BIOFABICS is primarily engaged in pre-clinical research.
In 2022, NASA, in collaboration with the National Institutes of Health (NIH), the Department of Health and Human Services Biomedical Advanced Research and Development Authority (BARDA), and the Food and Drug Administration (FDA), selected 8 research projects to enhance the longevity of 3D tissue chips to a minimum of 6 months. This multi-agency effort aimed to achieve tissue viability and physiological function extension through automated engineering capabilities, enabling real-time online readouts in complex human in vitro models, such as tissue chips or micro-physiological systems. The scientific objectives of this initiative included gaining deeper insights into disease models, facilitating drug development, optimizing clinical trial design, understanding chemical and environmental exposures and countermeasures, and investigating physiological changes induced by the spaceflight environment. Critical to the success of these endeavors is the in-depth characterization of tissue chips, particularly in distinguishing between acute and chronic exposures, marking a significant advancement in the evolution of these technologies.
The good news of the month: Rejuvenating Aged Immunity by Depleting Myeloid-Biased Stem Cells
Researchers of the University of Stanford (USA) found that depleting myeloid-biased hematopoietic stem cells (my-HSCs) in aged mice rejuvenated their immune systems, boosting lymphocyte progenitors, naive T cells, and B cells. This led to improved immune responses to viral infections, pointing to a potential approach to combat age-related immune decline and inflammation.
For more information