A.I. could double the human life span in five years. Dario Amadei, CEO of Anthropic, World Economic Forum in Davos, January 2025 (Source).
This month’s theme: Human clinical trials for longevity. International comparison.
The development of a new drug or therapy is a long and complex process. Before commercialisation, treatments must go through multiple phases of testing, including clinical trials, which assess their effectiveness, safety, and potential side effects. Clinical trials are essential for making the most innovative treatments accessible to the public or to specific patient groups. The legal frameworks for these trials are evolving rapidly and differ significantly between countries. Almost all human clinical trials are mentioned on the website clinicaltrials.gov.
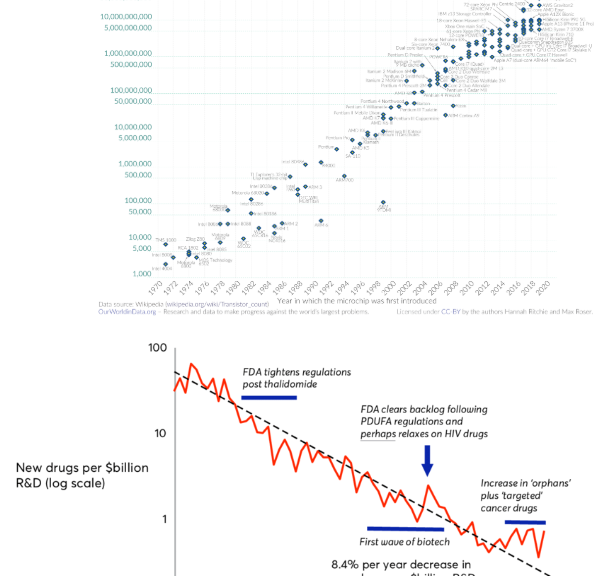
A human clinical trial is generally divided into 3 phases. Phase 1 proves innocuousness. Phase 2 proves efficiency on a small number of patients. Phase 3 proves efficiency on a large group. Human clinical trials generally follow tests on animals and precede the approval for use in a long and costly process. It is generally considered that the total price for the approval of one new drug is above one billion dollars and that the rate of discoveries is decreasing. This phenomenon is called Eroom’s law. The cost is due to the complicated rules, but also because many attempts to find a drug are failures.
For longevity-focused research, these legal developments are essential. By harmonizing authorization processes or expanding access to experimental treatments, countries can significantly accelerate progress in various fields such as regenerative medicine and gene therapies. Thus, faster trials would lead to faster access to innovations that prolong and improve life.
United States
In the United States, Montana has emerged as a hub for various types of clinical trials, including biohacking and experimental treatments. Thanks to a law adopted in 2023, known as the Right to Try, the state now allows experimental treatments to be offered to all types of patients, not just those with terminal illnesses. Before this law, patients needed FDA approval to access investigational drugs that had not yet been formally approved. This rule now allows patients who have exhausted standard treatments to try new therapeutic options. The Right to Try approach is not unique to Montana; it exists in most states.
In addition, the expansion of the right to try in Montana is attracting companies specializing in biotechnology and longevity. According to some, more than 20 biotechnology companies, particularly those specializing in regenerative medicine and anti-aging, are considering setting up shop in Montana to implement early access programs for patients.
However, it is important to note that the Right to Try only gives companies the opportunity to offer experimental treatments, without creating a legal obligation to do so. Patients cannot demand access to these treatments, and companies remain free to decide whether to offer them free of charge or at a cost.
Europe – European Union
In Europe, since 2022, as part of the « ACT EU » initiative, the Clinical Trial Regulation (CTR) has sought to harmonise clinical trial regulations across EU member states. To achieve this, the Clinical Trials Information System (CTIS) was introduced to centralise applications, simplify international procedures, increase transparency, and speed up approvals. The CTIS serves as a single entry point for clinical trial applications in all member States, replacing the complex set of national procedures that previously slowed down multinational clinical trials. Sponsors can now submit a single application for up to 30 EU/EEA countries at once, reducing delays and administrative work. As a result, since January 31, 2025, all European clinical trials have been following the CTIS system.
All submitted trials must comply with the Good Clinical Practice (GCP) standards to ensure patient safety.
The administrative approval process takes about 6 to 10 months in the US and approximately 7 months in Europe (210 days). In terms of costs, each phase of the clinical trials in the United States can cost between $1.4 million and over $100 million. The total development of a drug in the US typically costs between $1 billion and $2.6 billion, while in Europe, clinical trials tend to be less expensive overall, with a lower average cost per participant (approximately US$15,000 to US$25,000).
United Kingdom
The United Kingdom, like Europe, aims to re-establish itself as a leading hub for clinical research. Following Brexit, several reforms have been introduced. Starting in 2026, all clinical trials conducted in the country must follow international standards, particularly those of the International Council for Harmonisation (ICH), to ensure global recognition of trial data. Additionally, transparency will be increased: the researchers of every trial will be required to publish a plain-language summary of its results for public access.
Moreover, the UK is actively investing to become a global leader in clinical innovation. The UK government’s Recovery, Resilience and Growth (RRG) program, which brings together the MHRA, NHS, DHSC, NIHR, regulators, academia, and industry, is establishing a national guide to integrate research into all healthcare systems and reduce trial implementation times. To this end, more than £400 million will be invested to create up to 18 new commercial research centers (CRDCs) across the country, which will promote patient recruitment and strengthen clinical trial infrastructure. The government also plans to reduce the average time to start clinical trials from 250 days to just 10 weeks.
Australia
Australia is recognised for its high-quality clinical research, supported by robust regulations and internationally recognised standards. Like many leading countries, including the US and EU member states, Australia follows internationally established guidelines such as the Declaration of Helsinki and Good Clinical Practice (GCP) standards set by the ICH, ensuring participant safety, protecting their rights and well-being, and facilitating global recognition of the research. Australia is a leader in early-phase clinical trials, including first-in-human studies.
In addition, Australia offers several advantages that make it particularly attractive for research in the fields of biotechnology and longevity. The country has one of the fastest regulatory approval systems in the world, with many Phase I trials starting within weeks of submission.
Bahamas
Clinical research is also active in the Bahamas, particularly for stem cell-based therapies. Unlike in many countries, clinical trials there, regulated by the Bahamas National Stem Cell Ethics Committee, Good Clinical Practice, and local registration, can be funded directly by patients themselves. This model accelerates the pace of the research and provides more flexibility for experimental therapies.
China
China has seen a sharp increase in clinical trials and their development in recent years. In fact, by 2023, the number of trials conducted in China had surpassed those in the United States. This acceleration is reflected in the data: that year, China conducted more than 14,000 active clinical trials.
Since 2015, the Chinese government has implemented several reforms, including its own Good Clinical Practice (GCP) guidelines, to facilitate research and reduce the approval timeline for new drugs to 60 days. These efforts bring China closer to ICH standards, enabling greater participation in international trials and smoother integration of Chinese-developed treatments abroad.
However, some studies raise concerns about the reliability of Chinese clinical trials, pointing to ongoing quality and ethical challenges in certain areas of research.
Private zones – The example of Prospera
In response to highly restrictive regulations, private experimental zones are also emerging. One such example is Prospera, located on Roatán Island in Honduras. Prospera adopts a libertarian approach to clinical research, offering a regulatory framework with shorter approval times and lower costs compared to traditional authorities like the FDA. It is home to several biotech clinics, such as MiniCircle, which conducts gene therapy trials for muscle regeneration and metabolic health.
However, critics warn of insufficient legal, ethical and patient protection frameworks in these environments.
Conclusion
The global clinical trial landscape is changing. From Montana’s “Right to Try” laws to harmonized EU regulations, from Australia’s first human studies to China’s rapid expansion, many countries are shaping the speed and safety with which new therapies reach patients. And there are other interesting developments that we will not approach in this newsletter in India, Japan, Mexico, … Considering the importance of the USA and the European Union for the development of new therapies, it is to be hoped that clinical trials will follow good examples of other countries or make approvals of therapies really easy when good clinical trials are made outside of their borders. All other things being equal, going faster saves lives directly and also indirectly by accelerating research/
For those invested in longevity, understanding these changes is important; it provides insight into the areas where the next breakthroughs will emerge and how quickly they could transform human health and well-being.
To accelerate clinical trials for longevity, we also need more people volunteer for themselves and for the community. We will approach this in one of the next newsletters.
The good news of the month. ARPA-H Project concerning the brain.
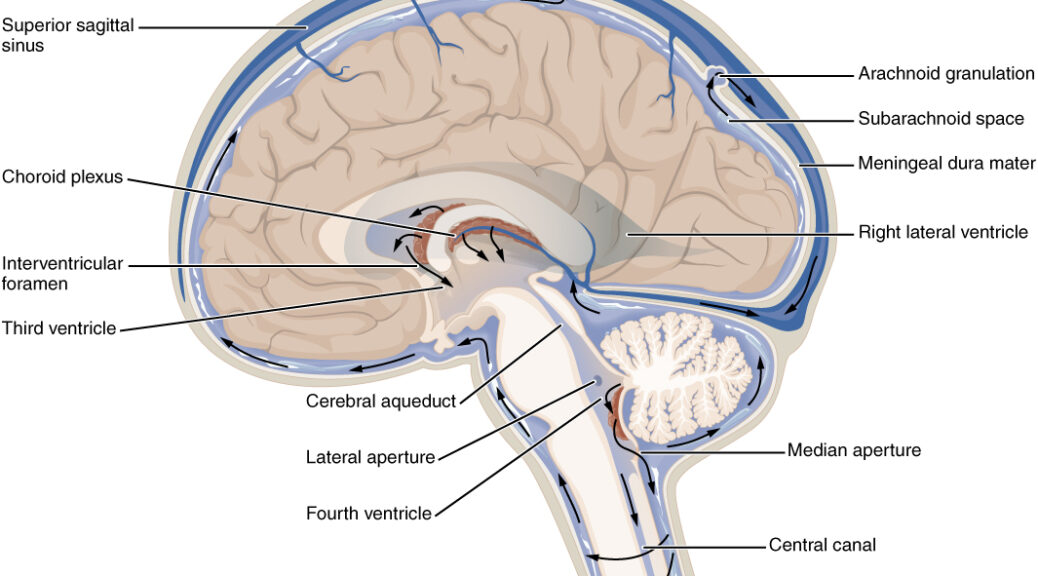
The ARPA-H (Advanced Research Projects Agency for Health) has launched the FRONT (Functional Repair of Neocortical Tissue) program, which aims to restore brain function in people who have suffered permanent damage to the neocortex. This program aims to regenerate damaged brain tissue by using unspecialized cells transformed into functional cortical tissue to restore lost cognitive functions. This is important and promising concerning Alzheimer’s disease. The goal is to reduce the costs associated with long-term care and improve patient autonomy. ARPA-H is inviting researchers to submit proposals for August-September 2025.
For more information